Study: Social factors keep women from getting mammograms
Published 4:47 pm Friday, April 19, 2024
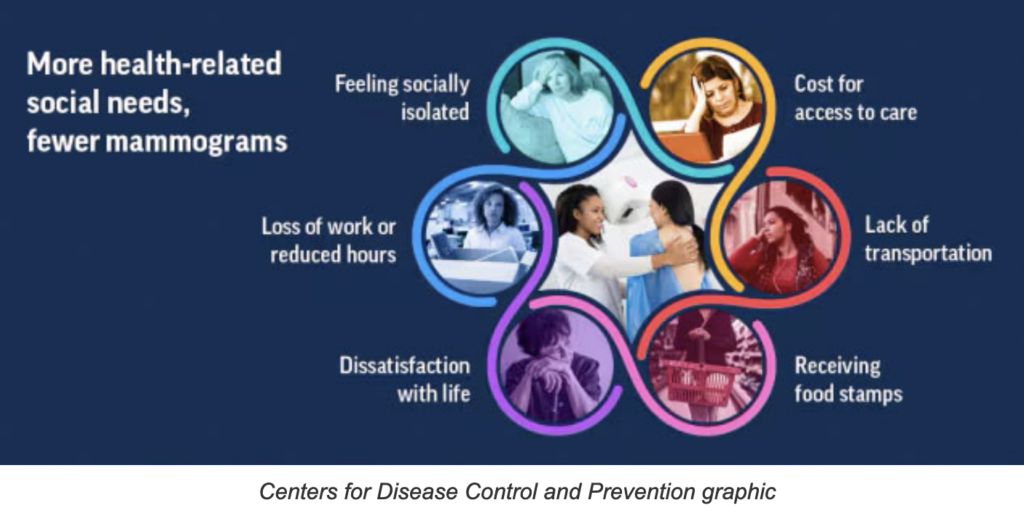
- (CDC graphic)
A Centers for Disease Control and Prevention study says the more health-related social needs a woman has, the less likely she is to get a mammogram.
The study defines health-related social needs, or HRSNs, as social conditions that adversely affect a person’s health. Examples include feeling socially isolated, loss of work or reduced hours, dissatisfaction with life, the cost to access health care, a lack of transportation, and receiving food stamps. HRSNs are some of the social determinants of health.
Using data from the CDC’s 2022 Behavioral Risk Factor Surveillance System, a continuing national survey, the researchers found that mammogram use was almost 20% lower among women between the ages of 50 and 74 who had three or more HRSNs, compared to women who had no such needs.
The report did not provide state-level data, but health-related social needs are more prevalent in Kentucky than in most states
In Kentucky, 59% of women aged 40-49 and and 72% of women aged 50-74 reported having had a mammogram within the previous two years, according to the 2022 BRFSS data. The rate for younger women 40-49 was the same as the national average, but the rate for those 50-74 was 4.6 percentage points less.
Among U.S. women aged 50 to 74 with no adverse HRSNs, 83 percent had a mammogram in the last two years, while that was true for only 66 percent of those with three or more adverse HRSNs.
“We have to address these health-related social needs to help women get the mammograms they need,” Dr. Debra Houry, chief medical officer at the CDC, said in a news release. “Identifying these challenges and coordinating efforts between health care, social services, community organizations, and public health to help address these needs could improve efforts to increase breast cancer screening and ultimately save these tragic losses to families.”
Breast cancer causes more than 40,000 deaths in U.S. women each year, according to the news release.
Between 2016 and 2020, Kentucky’s breast-cancer rate was 126.7 per 100,000 people and its breast cancer death rate was 21.6 per 100,000, according to the National Cancer Institute State Cancer Profiles. The national rate was 19.6.
The report adds that Black women and women of lower socioeconomic status are more likely to die from breast cancer.
The U.S. Preventive Services Task Force currently recommends that women aged 50 to 74 get a screening mammogram every two years and that women ages 40 to 49 talk to their health-care providers about when to start and how often to get a mammogram.
Most health-insurance plans cover the full cost of screening mammograms, but follow-up diagnostic imaging is not always covered.
To address this, Kentucky lawmakers recently passed House Bill 115, which eliminates co-payments and cost-sharing requirements for high-risk individuals who need follow-up diagnostic imaging to rule out breast cancer. Gov. Andy Beshear signed HB 115 into law on April 5. It takes effect Jan. 1, 2025.
“Thousands of Kentuckians require diagnostic and supplemental breast imaging every year, yet many forgo them due to out-of-pocket costs. Not anymore,” Molly Guthrie, vice president of policy and advocacy at the breast-cancer foundation Susan G. Komen, said in a news release. “This life-saving legislation means they will now receive the breast imaging they require, leading to an earlier breast cancer diagnosis and often better health outcomes.”






